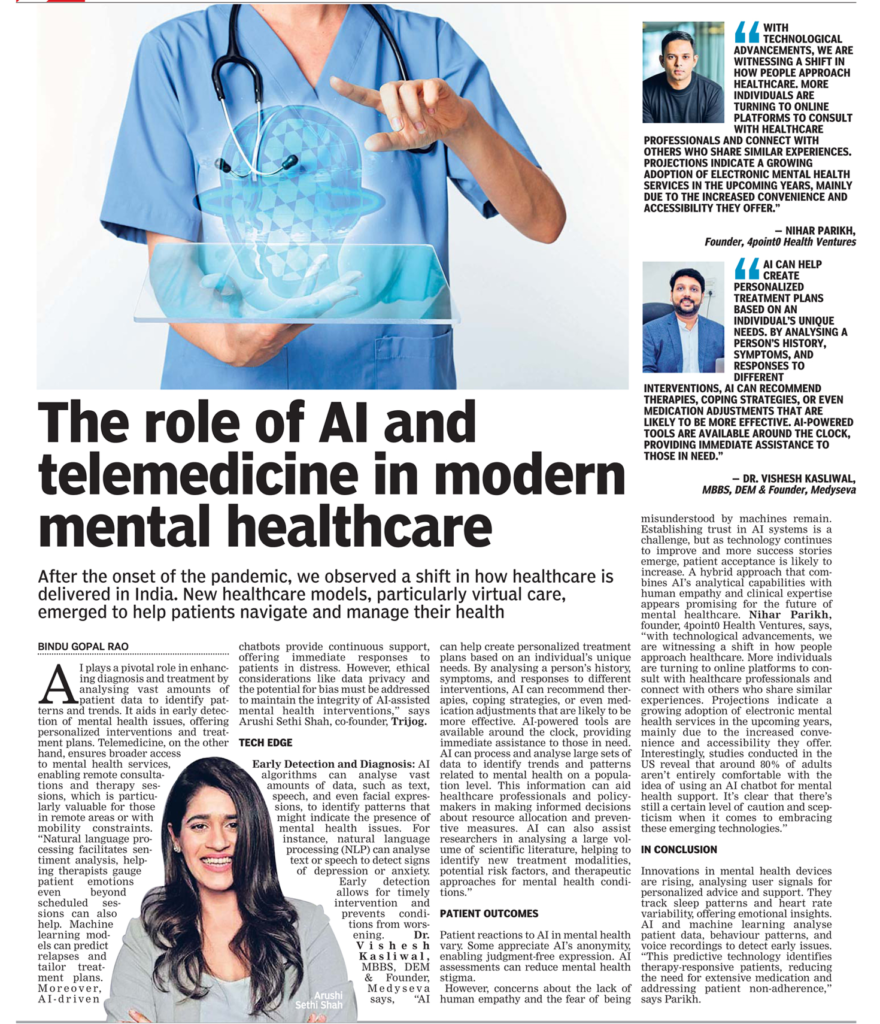
AI and telemedicine play significant roles in modern mental healthcare. AI technologies can assist in diagnosing mental health conditions, monitoring patient progress, and even offering personalized therapeutic interventions. Telemedicine, on the other hand, enables remote consultations, providing easier access to mental health professionals and reducing barriers like distance and stigma. Together, AI and telemedicine enhance the efficiency, accessibility, and effectiveness of mental healthcare by leveraging technology to reach a wider range of individuals and provide tailored support.
AI can help track an individual’s progress over time by analysing data from various sources, such as wearable devices and self-reporting apps. This allows therapists to assess the effectiveness of treatment plans and adjust as needed. AI-powered interactions can create a private space where people can discuss their concerns openly.
Natural Language Processing (NLP): NLP enables AI to understand and respond to human language, making it useful in virtual therapy sessions, mental health chatbots, and sentiment analysis. It allows AI to pick up on emotional cues and offer appropriate responses.
In essence, AI’s strength lies in its ability to process and analyse data at a scale and speed that humans cannot achieve alone. This capacity enhances the accuracy of diagnoses, the personalization of treatment, and the accessibility of mental healthcare, ultimately leading to better outcomes for individuals seeking support for their mental well-being.
Patients’ reactions to the concept of using AI in mental healthcare can vary widely based on factors such as personal preferences, comfort with technology, and the nature of their mental health condition. Here are some common reactions:
Many patients are curious about AI’s potential benefits and are open to trying new technological approaches to manage their mental health. They may see AI tools as a complement to traditional therapy and appreciate the convenience and accessibility they offer.
Some patients may be sceptical about the effectiveness of AI in addressing complex emotional and psychological issues. They might worry that AI lacks the empathy and understanding that human therapists provide, or they might be concerned about privacy and data security.
Patients who face barriers to accessing in-person mental health services, such as geographical limitations or social stigma, might feel relieved that AI-powered solutions provide more accessible and discreet avenues for support.
Individuals who are accustomed to traditional therapy models might resist the idea of incorporating AI into their treatment. They might prefer the familiar dynamics of in-person sessions and view AI as a departure from their comfort zone.
Many patients find value in using AI tools as a complement to traditional therapy. They may see AI to practice coping techniques, receive immediate support during challenging moments, or track their progress over time.
Younger patients who are more familiar with technology might be more receptive to the idea of AI in mental healthcare, while older individuals might take longer to adapt to these concepts. It is important for mental health professionals to approach the integration of AI with sensitivity, offering patients clear information about the benefits, limitations, and potential role of AI in their treatment journey.
The use of AI in mental health raises important ethical questions, such as data privacy, informed consent, and the potential for AI to unintentionally reinforce biases. Ensuring that AI algorithms are transparent, unbiased, and respectful of users’ privacy is crucial.
While AI can be a powerful tool, it should not replace the role of human mental health professionals. Human oversight is essential to ensure that AI-generated recommendations align with the individual’s unique context and needs.
As AI technology continues to advance, it’s important to monitor the long-term impact of AI interventions on patients’ well-being. Research should focus on understanding how sustained use of AI tools affects mental health outcomes.
AI tools should be culturally sensitive and consider diverse perspectives. Mental health experiences and expressions can vary greatly across cultures, and AI should be adaptable to different cultural contexts.
Patients should be educated about the capabilities and limitations of AI tools in mental healthcare. Clear communication about how AI can complement their treatment and what to expect from AI interactions can help manage expectations.
The most effective approach often involves integrating AI tools with traditional mental healthcare practices. This could mean using AI for continuous monitoring, progress tracking, and providing supplementary support between in-person therapy sessions.
The effectiveness of AI tools in mental health should be rigorously researched and validated through clinical trials and studies. Evidence-based practices will help build trust in the field and guide the responsible use of AI.
AI algorithms should be continuously refined and improved based on user feedback and evolving research. This ensures that the technology remains relevant, effective, and aligned with users’ needs.
AI tools should empower users by providing them with insights, tools, and information that allow them to take an active role in their mental health journey. This can lead to better engagement and more positive outcomes.
The development and deployment of AI in mental healthcare should adhere to ethical guidelines and regulatory standards to ensure patient safety and well-being.
AI interventions should be customizable to accommodate individual preferences and evolving needs. A one-size-fits-all approach may not be effective in addressing the diverse range of mental health conditions and experiences.
As AI technology continues to evolve and be integrated into mental healthcare practices, ongoing collaboration between mental health professionals, technologists, researchers, and patients will be crucial to ensure that AI is used responsibly and effectively to support mental well-being.
AI and telemedicine have the incredible potential to address this, especially given the scarcity of registered psychiatrists and psychologists in the country. The numbers speak for themselves – around 130 million individuals require mental health services, yet the availability of professionals remains alarmingly low, with just 0.75 psychiatrists per 100,000 population compared to the global median of 3. Telemedicine and teleconsultation can bridge the geographical divide between patients and mental health professionals. This not only enhances access but also has the potential to significantly reduce the cost of consultation for patients.
India’s current healthcare landscape is also seeing the emergence of useful technologies in mental health, including teletherapy, mental health apps, virtual reality tools, and AI-driven chatbots. These innovations are making mental healthcare more accessible, confidential, and affordable. Moreover, they contribute to fostering a supportive community for those seeking help.
By leveraging AI, healthcare companies can make a meaningful impact on people’s lives and enhance patient outcomes across various mental health conditions. Take chatbots, for example. They’re increasingly being used to provide guidance and 24×7 support for individuals undergoing mental health treatment. These chatbots help people cope with their symptoms and can identify important keywords that might indicate the need for direct communication with a human mental health professional.
Read the full story that first appeared in Deccan Herald dated Sep 27, 2023 here: