
Technology is changing not just how diabetes is being treated but also managed by doctors and patients alike.
Ask any diabetic person what irks them most about their health condition and the answer that you would most likely receive is monitoring their sugar levels in real time so that they can lead as normal a life as anyone else would. As a lifestyle disease that is all about management, eating right, exercising and regular health checks, diabetes needs the patient to be in control to stay ahead of the issue. Today however a lot of this is changing thanks to technological innovations that help patients take charge to manage diabetes better than before. In fact this includes the whole realm from diagnostics to treatment to detection and management.
New vistas
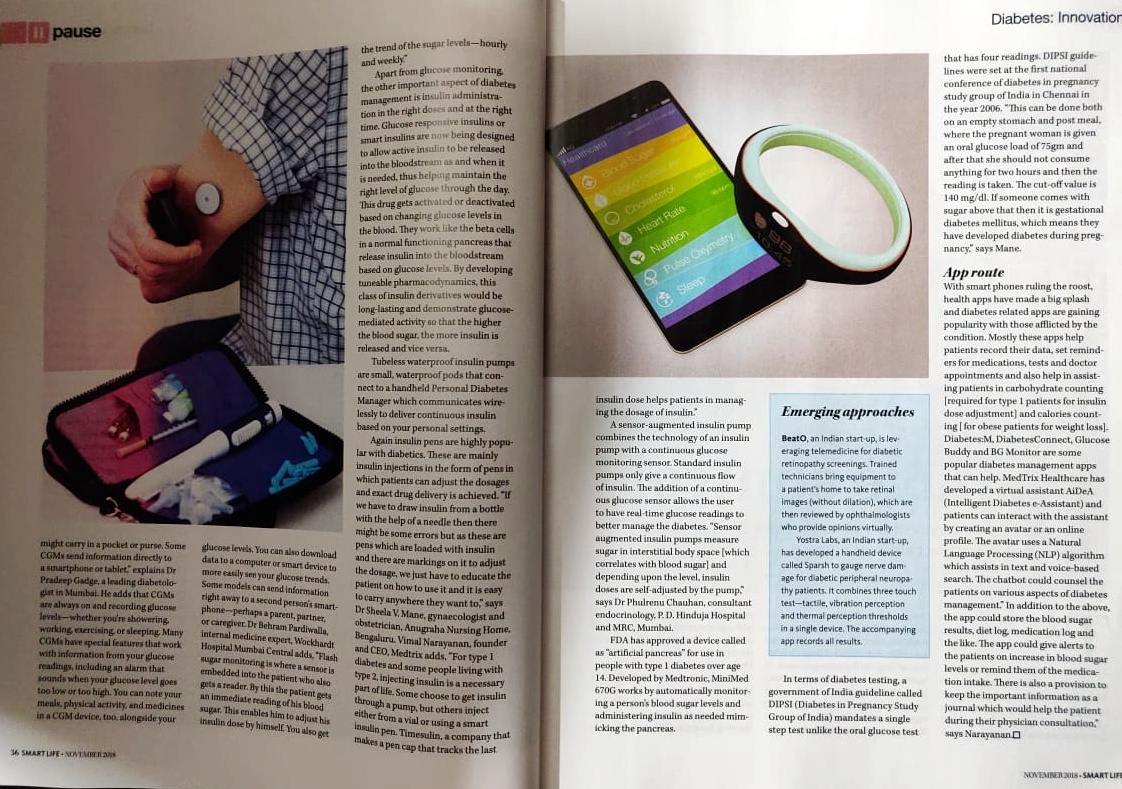
Some of the new technologies include continuous glucose monitors that are inserted on patients arm and back and continuously measure blood sugar at five minute interval. Continuous glucose monitor (CGM) provide real time (actual) information about current blood glucose, short term feedback about effectiveness of diabetes interventions and warning about hypo or hyperglycemi. “CGM works through a tiny sensor inserted under your skin, usually on your belly or arm. The sensor measures your interstitial glucose level, which is the glucose found in the fluid between the cells. The sensor tests glucose every few minutes. A transmitter wirelessly sends the information to a monitor. The monitor may be part of an insulin pump or a separate device, which you might carry in a pocket or purse. Some CGMs send information directly to a smartphone or tablet. A transmitter sends data to a receiver. The CGM receiver may be part of an insulin pump or a separate device,” says Dr Pradeep Gadge, Diabetologist, Gadge Diabetes Centre, Mumbai. CGMs are always on and recording glucose levels—whether you’re showering, working, exercising or sleeping. Many CGMs have special features that work with information from your glucose readings including an alarm can sound when your glucose level goes too low or too high. You can note your meals, physical activity, and medicines in a CGM device, too, alongside your glucose levels. You can download data to a computer or smart device to more easily see your glucose trends. Some models can send information right away to a second person’s smartphone—perhaps a parent, partner, or caregiver. For example, if a child’s glucose drops dangerously low overnight, the CGM could be set to wake a parent in the next room. Glucose responsive insulins or smart insulins are being designed to allow active insulin to be released into the bloodstream as and when it is needed. By developing tuneable pharmacodynamics, this class of insulin derivatives would be long-lasting and demonstrate glucose-mediated activity so that the higher the blood sugar, the more insulin is released and vice versa.
Insulin Pumps
Tubeless waterproof insulin pumps that are small, waterproof pods and the handheld Personal Diabetes Manager communicate wirelessly to deliver continuous insulin based on your personal settings. Vimal Narayanan, founder and CEO, Medtrix says, “For type 1 diabetes and some people living with type 2, injecting insulin is a necessary part of life. Some choose to get insulin through a pump, but others inject either from a vial or using a smart insulin pen. Timesulin, a company that makes a pen cap that tracks the last insulin dose help patients in managing the dosage of insulin.” Dr Behram Pardiwalla, internal medicine expert, Wockhardt Hospital Mumbai Central adds, “Flash sugar monitoring is where a sensor is embedded into the patient who also gets a reader. By this the patient gets an immediate reading of his blood sugar. This enables him to adjust his insulin dose by himself. You also get the trend of the sugar levels – hourly and weekly.”
A sensor-augmented insulin pump combines the technology of an insulin pump with a continuous glucose monitoring sensor. Standard insulin pumps only give a continuous flow of insulin. The addition of a continuous glucose sensor allows the user to have real-time glucose readings to better manage the diabetes. “Sensor augmented insulin pumps that measure sugar in interstitial body space [which correlates with blood sugar] and depending upon the level insulin doses are self-adjusted by pump are also being seen,” says Dr Phulrenu Chauhan, consultant endocrinology, P. D. Hinduja Hospital & MRC, Mumbai. Today for those who are insulin dependent diabetic, instead of using insulin pumps, there are insulin injections in the style of pens where they can adjust their dosages on that accordingly and then they can shoot it and in using these pens the exact drug delivery happens. “Suppose if we have to draw insulin from a bottle with the help of a needle then there might be some errors but as these are pens which are loaded with insulin and there are markings on it to adjust the dosage, we just have to educate the patient on how to use it and it is easy to carry it anywhere they want to,” says Dr Sheela V. Mane, gynaecologist and obstetrician, Anugraha Nursing Home, Bengaluru.
FDA has approved a device called as “artificial pancreas” for use in people with type 1 diabetes over age 14. Developed by Medtronic, MiniMed 670G works by automatically monitoring a person’s blood sugar levels and administering insulin as needed mimicking the pancreas, the organ in our bodies that in healthy people is able to moderate blood sugar levels by pumping out insulin that can process the sugars in food. Currently, the MiniMed 670G system is only available in the US, but they have recently received CE Mark approval for our European customers. However, the company have not confirmed when the product would be available in India.
Taking charge
Today it is a Government of India guideline which earlier was called DIPSI – Diabetes in Pregnancy Study Group of India, where a single step test is done unlike the oral glucose test that has four readings. DIPSI guidelines were set at the first national conference of diabetes in pregnancy study group of India in Chennai in the year 2006. “This can be done both on an empty stomach and post meal, where she is given a load of 75grams and after that she should not consume anything for two hours and then the reading is taken. The cut-off value is 140 mg/dl. If someone comes with sugar above that then it is gestational diabetes mellitus, which means they have developed diabetes during pregnancy,” says Dr. Mane.
App Route
With smart phones ruling the roost, health apps have made a big splash and diabetes related apps are gaining popularity with those afflicted by the condition. Mostly these apps help patients record their data, set reminders for medications, tests and doctor appointments and also help in assisting patients in carbohydrate counting [required for type 1 patients for insulin dose adjustment] and calories counting [for obese patients for weight loss]. Diabetes:M, DiabetesConnect, Glucose Buddy and BG Monitor are some popular diabetes management apps that can help too. MedTrix Healthcare has developed a virtual assistant AiDeA (Intelligent Diabetes e-Assistant) that is powered by IBM Watson (Artificial Intelligence). The patients can interact with the app through an online profile. In addition to the above, the app could store the blood sugar results, diet log, medication log and the like. The app could give alerts to the patients on increase in blood sugar levels or remind them of the medication intake. There is also a provision to keep the important information as a journal which would help the patient during their physician consultation,” says Narayanan. Now how is that to add a tech dimension to control your diabetes?
Emerging Approaches
- BeatO, an Indian start-up, is leveraging telemedicine for diabetic retinopathy screenings. Trained technicians bring equipment to a patient’s home to take retinal images (without dilation), which are then reviewed by ophthalmologists who provide opinions virtually.
- Yostra Labs, an Indian start-up, has developed a handheld device called Sparsh to gauge nerve damage. It combines 3 touch test, tactile, vibration perception, thermal perception thresholds in a single device; the accompanying app records all results.

Leave a Reply